Stage 3 Bedsores
- Reviewed By
Anthony C. Lanzone, Founding Partner
Stage 3 bedsores are deep wounds that can lead to severe complications, including infections, sepsis, and death. They require urgent treatment that can last months, years, or a lifetime. They are almost always preventable, and nursing home negligence is the primary cause.
A stage 3 bedsore is a deep sore that penetrates all three layers of the skin down to the body fat. They carry a high risk of dangerous and potentially deadly complications, including septic shock. Also known as pressure injuries, pressure sores, pressure ulcers, or decubitus ulcers, bedsores are preventable injuries that often occur because nursing home staff fail to reposition residents and keep their skin clean and dry.
If your loved one has developed a stage 3 bedsore in a nursing home, they may be entitled to substantial compensation through a nursing home abuse lawsuit. Our experienced nursing home abuse lawyers can seek to hold the nursing home accountable for your loved one’s losses. Call (888) 887-9777 today for a free consultation.
Table of Contents:
- What Does It Mean if a Bedsore is Stage 3?
- Stage 3 Bedsore Symptoms and Signs
- Why Stage 3 Pressure Injuries Are Challenging To Diagnose
- How Long Does It Take a Stage 3 Bedsore To Heal?
- What Is the Life Expectancy for Someone with a Stage 3 Pressure Ulcer?
- Causes of Stage 3 Bedsores
- Prevention
- Recovering Compensation for Stage 3 Pressure Ulcer Injuries
What Does It Mean if a Bedsore Is Stage 3?
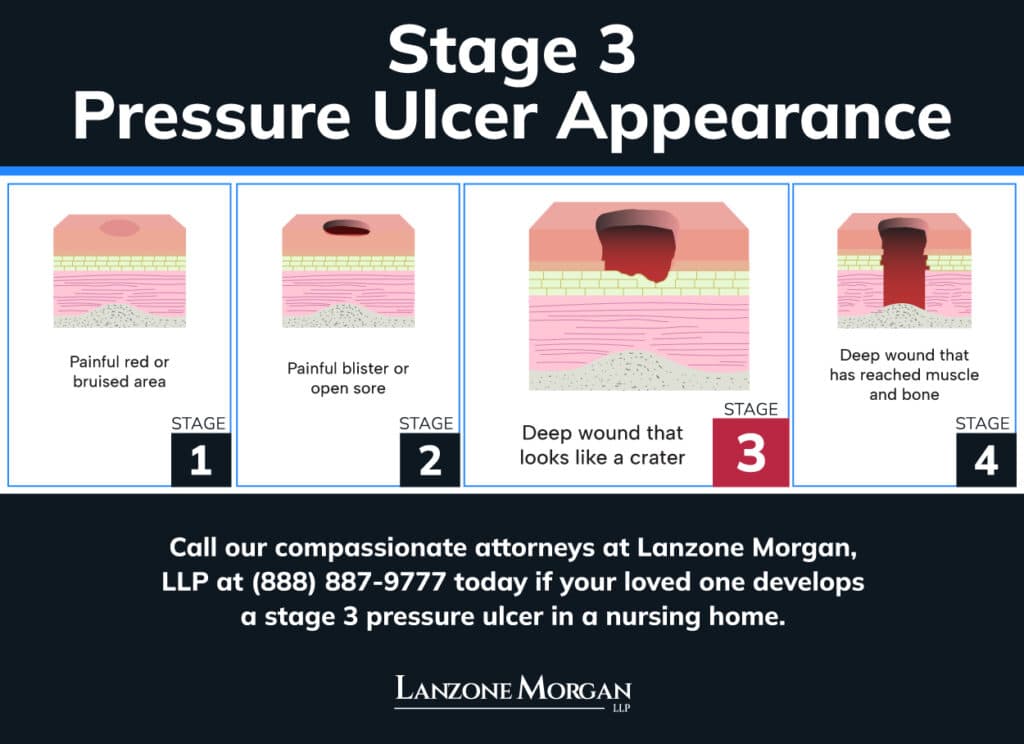
There are four stages of bedsores. Stage 3 bedsores are full-depth wounds that impact the epidermal and dermal layers of the skin, down to the fatty layer. They provide an easy pathway for harmful bacteria to enter the body and reach the blood or bones.
Stage 3 Bedsore Symptoms and Signs
A stage 3 pressure ulcer is a deep sore that presents with the following signs and symptoms:
- A deep, crater-like sore surrounded by dark skin
- Visible fatty tissue at the bottom of the sore
- Narrow tunnels leading deeper into the tissue
- Pockets under the surrounding skin
- Dead tissue that may be white and moist or dark and hard
- Severe pain, except in patients with nerve damage
- Clear, bloody, or pus-like drainage from the wound
- Redness, warmth, and swelling in the immediate area
- Foul odor, particularly if dead tissue is present
- Blisters that break and deepen the wound
Common Locations for Stage 3 Bedsores
Most bedsores develop on areas where bones protrude and press against the patient’s bed or chair for an extended period. The following are the most common sites where bedsores develop:
- Tailbone
- Buttocks
- Hip bones
- Back of the head
- Shoulder blades
- Elbows
- Heels
- Outer ankle bones
- Shoulders
- Ears
Why Stage 3 Pressure Injuries Are Challenging To Diagnose
Stage 3 pressure sores can be difficult to diagnose if they contain a large amount of dead tissue. Eschar is dead tissue with a dark, dry, scab-like appearance, while slough is moist, slimy, and pus-like dead tissue. Both types can disguise the depth of the wound, making it impossible to determine whether it is a stage 3 or 4 bedsore. Thus, these bedsores are unstageable.
Stage 3 pressure ulcers can also be confused with other conditions, including the following:
- Diabetic ulcers
- Venous ulcers
- Pyoderma gangrenosum, an autoimmune condition
Misdiagnosing a stage 3 bedsore can prevent a patient from getting the appropriate treatment and make it worse.
How Long Does It Take a Stage 3 Bedsore To Heal?
It can take a stage 3 bedsore weeks to months to heal, and sometimes longer, depending on the patient’s comorbidities, weight, age, overall health, and the type of treatment used.
Studies show that 50% of stage 3 pressure ulcers heal within six months. Some pressure injuries never heal if complications develop or the patient has severe comorbidities.
Treatment for Stage 3 Pressure Injuries
Nursing homes that fail to prevent bedsores are tasked with a significantly higher level of care to treat them, particularly when they reach stage 3. An effective treatment plan must include the following:
- Pressure relief: Pillows, cushions, low-pressure mattresses, and positioning that takes pressure off the wound
- Debridement: Dead tissue removal by facilitating the body’s natural processes, manually scraping it away, or using surgical instruments.
- Wound dressings: Dressings moistened with hydrogel, alginate, foam, hydrocolloid, or saline-soaked gauze
- Wound disinfection: Wound cleaning every time dressings are changed
- Antibiotics: Topical antibiotics if no improvement within 14 days, and systemic antibiotics if no improvement in two to four weeks or infections develop
- Reconstructive surgery: Direct closure, skin grafts, and skin flaps when other treatments are ineffective
- Pain management: Pain assessments, debridement, and dressing changes, with topical or systemic pain medication as needed
Stage 3 Pressure Ulcer Complications
Stage 3 pressure ulcers carry a high risk of serious complications, including the following:
- Osteomyelitis, a bone infection
- Cellulitis, an infection of the deep layers of the skin
- Septic arthritis
- Sepsis and septic shock
- Loss of body protein and dehydration from wound drainage
- Chronic anemia and abnormal protein accumulations in the organs
- Gangrene, tissue death that can spread to surrounding tissues or the blood
- Amputation of the foot or leg
- Death from complications
What Is the Life Expectancy for Someone with a Stage 3 Pressure Ulcer?
Older patients with bedsores have a 260% increased risk of death within 21 months, according to medical research. However, not all of the risk is directly attributable to bedsores since most patients who develop them have poor overall health with multiple comorbidities.
Infected bedsores can lead to serious infections, including sepsis, which dramatically reduces life expectancy. Sepsis from a pressure injury carries a high risk of death within 28 days.
Negligent management of a stage 3 pressure wound increases the risk of sepsis. Nursing homes can be held accountable for deaths that stem from negligent pressure injury care.
Causes of Stage 3 Bedsores
Bedsores occur when the skin breaks down because of prolonged pressure in bony areas, especially when combined with constant moisture.
Friction and shear also contribute to skin breakdown. Shear occurs when the skin is pulled in opposite directions, most notably when a resident sits in a bed in an inclined position. Nursing home staff often contribute to bedsore formation by doing the following:
- Leaving immobile residents in the same position for too long
- Letting residents wet or soil themselves instead of helping them get to the restroom
- Leaving residents in wet or soiled clothing for hours
- Ignoring bedsores at earlier stages and allowing them to progress
A stage 3 bedsore that develops in a nursing home is almost always a sign of neglect. Contact our knowledgeable California nursing home abuse lawyers immediately if your loved one is diagnosed with a stage 3 bedsore in a nursing home.
Prevention
Nursing homes can almost always prevent bedsores from developing. It requires a proactive approach with attentive care.
Assess the Risk
Nursing homes should perform skin assessments at admission and on a weekly basis thereafter for residents at risk of developing bedsores. Residents with the following conditions have the highest risks:
- Lack of mobility
- Conditions that affect circulation, such as diabetes
- Bowel or bladder incontinence
- Multiple chronic conditions
- Malnutrition and dehydration
- Loss of sensation from nerve damage
Pressure Relief
Nursing home staff should reposition bedridden residents at least every two hours and avoid placing their beds in incline positions that pull the skin on the tailbone or buttocks. Pressure-relieving mattresses, cushions, and pads can also prevent bedsores from developing or worsening, especially when a resident’s risk is high.
Good Hygiene
Constant moisture and acids from urine and feces promote skin breakdown and increase the risk of bedsores. Nursing home staff can mitigate the risk by helping continent residents use the bathroom as needed and promptly changing the diapers, clothing, and linens of incontinent residents.
Proper Nutrition and Hydration
Nursing staff should be aware of the amount of food and fluids each resident consumes. They should monitor residents’ weight, provide feeding assistance as needed, and report unexplained weight loss to the physician.
Staff Training
All staff should have a thorough working knowledge of the risk factors for bedsores, their appearance, the stages, prevention, and proper care. CNAs should be able to recognize the signs of pressure ulcers and understand the importance of reporting them promptly.
Manage Chronic Conditions
Chronic conditions like diabetes and peripheral artery disease affect circulation and make residents more susceptible to pressure ulcers. Proper management of these conditions is crucial for maintaining good blood flow, preventing nerve damage, and facilitating wound healing.
Recovering Compensation for Stage 3 Pressure Ulcer Injuries
Stage 3 bedsores are serious nursing home injuries that should never occur. Bedsores bring on months or years of suffering and medical treatment. If your loved one has a stage 3 bedsore, you may be entitled to economic and non-economic damages for you and your loved one’s losses, including the following:
- Current and future medical expenses
- Lost wages you experienced while protecting your loved one
- The cost of moving your loved one
- Pain and suffering
- Emotional distress
- Humiliation and loss of dignity
- Loss of bodily functions
We have recovered over $200 million in settlements and verdicts, including a recent bedsore settlement of $3 million. Your loved one deserves quality care. Contact us online or call (888) 887-9777 today, and let us get your loved one the justice they deserve.

- Fact-Checked
This content has been legally reviewed and approved by nursing home abuse attorney, Anthony Lanzone. Anthony holds notable memberships with professional organizations including the American Association for Justice and Consumer Attorneys of California.
VIEW SOURCES
Ahmed, S. R., Kotp, M. H., Hafez, A. A., Aly, M. A., Ismail, H. A., Bassiony, H. A., Attia, A. S., Mekdad, A. K., & Ahmed, R. K. (2025). Nurses’ performance regarding use of the Braden scale for predicting pressure ulcers among critically ill patients: self-learning package. BMC Nursing, 24(1). https://doi.org/10.1186/s12912-025-03511-0
Awad, S. S., Stern, J. D., Milne, C. T., Dowling, S. G., Sotomayor, R., Ayello, E. A., Aguirre, L. J. F., Khalaf, B. Z., Gould, L. J., Desvigne, M. N., & Chaffin, A. E. (2023). Surgical Reconstruction of Stage 3 and 4 Pressure Injuries: A Literature Review and Proposed Algorithm from an Interprofessional Working Group. Advances in Skin & Wound Care, 36(5), 249–258. https://doi.org/10.1097/01.asw.0000922708.95424.88
Bedsores. (2024, March 19). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/bedsores
Bluestein, D., & Javaheri, A. (2008, November 15). Pressure ulcers: Prevention, evaluation, and management. AAFP. https://www.aafp.org/pubs/afp/issues/2008/1115/p1186.html/1000
Mervis, J. S., & Phillips, T. J. (2025, September 8). Pressure sores. Merck Manual Consumer Version. https://www.merckmanuals.com/home/skin-disorders/pressure-sores/pressure-sores
Noie, A., Jackson, A. C., Taheri, M., Sayadi, L., & Bahramnezhad, F. (2024). Determining the frequency of pressure ulcers incidence and associated risk factors in critical care patients: A 3‐year retrospective study. International Wound Journal, 21(11). https://doi.org/10.1111/iwj.70120
Roderman, N., Wilcox, S., & Beal, A. (2024). Effectively addressing Hospital-Acquired Pressure injuries with a multidisciplinary approach. HCA Healthcare Journal of Medicine, 5(5). https://doi.org/10.36518/2689-0216.1922
Storm, J. (n.d.). Understanding Stage 3 pressure ulcers: causes, symptoms, treatment, and prevention. Quality Insights. https://www.qualityinsights.org/nursing-home-insights/understanding-stage-3-pressure-ulcers-causes-symptoms-treatment-and-prevention
Sugiyama, K., Tsuboya, T., Nakagawa, S., Kikuchi, T., & Tanoue, Y. (2024). Amputation-free Home Management of Infected Lower Extremity Pressure Ulcer through Shared Decision-making: Enhancing the Quality of Life and Highlighting Societal Significance in Home Care. Internal Medicine. https://doi.org/10.2169/internalmedicine.2881-23
Zaidi, S. R. H., & Sharma, S. (2024, January 3). Pressure ulcer. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK553107/

- Fact-Checked
This content has been legally reviewed and approved by nursing home abuse attorney, Anthony Lanzone. Anthony holds notable memberships with professional organizations including the American Association for Justice and Consumer Attorneys of California.
VIEW SOURCES
Ahmed, S. R., Kotp, M. H., Hafez, A. A., Aly, M. A., Ismail, H. A., Bassiony, H. A., Attia, A. S., Mekdad, A. K., & Ahmed, R. K. (2025). Nurses’ performance regarding use of the Braden scale for predicting pressure ulcers among critically ill patients: self-learning package. BMC Nursing, 24(1). https://doi.org/10.1186/s12912-025-03511-0
Awad, S. S., Stern, J. D., Milne, C. T., Dowling, S. G., Sotomayor, R., Ayello, E. A., Aguirre, L. J. F., Khalaf, B. Z., Gould, L. J., Desvigne, M. N., & Chaffin, A. E. (2023). Surgical Reconstruction of Stage 3 and 4 Pressure Injuries: A Literature Review and Proposed Algorithm from an Interprofessional Working Group. Advances in Skin & Wound Care, 36(5), 249–258. https://doi.org/10.1097/01.asw.0000922708.95424.88
Bedsores. (2024, March 19). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/bedsores
Bluestein, D., & Javaheri, A. (2008, November 15). Pressure ulcers: Prevention, evaluation, and management. AAFP. https://www.aafp.org/pubs/afp/issues/2008/1115/p1186.html
Mervis, J. S., & Phillips, T. J. (2025, September 8). Pressure sores. Merck Manual Consumer Version. https://www.merckmanuals.com/home/skin-disorders/pressure-sores/pressure-sores
Noie, A., Jackson, A. C., Taheri, M., Sayadi, L., & Bahramnezhad, F. (2024). Determining the frequency of pressure ulcers incidence and associated risk factors in critical care patients: A 3‐year retrospective study. International Wound Journal, 21(11). https://doi.org/10.1111/iwj.70120
Roderman, N., Wilcox, S., & Beal, A. (2024). Effectively addressing Hospital-Acquired Pressure injuries with a multidisciplinary approach. HCA Healthcare Journal of Medicine, 5(5). https://doi.org/10.36518/2689-0216.1922
Storm, J. (n.d.). Understanding Stage 3 pressure ulcers: causes, symptoms, treatment, and prevention. Quality Insights. https://www.qualityinsights.org/nursing-home-insights/understanding-stage-3-pressure-ulcers-causes-symptoms-treatment-and-prevention
Sugiyama, K., Tsuboya, T., Nakagawa, S., Kikuchi, T., & Tanoue, Y. (2024). Amputation-free Home Management of Infected Lower Extremity Pressure Ulcer through Shared Decision-making: Enhancing the Quality of Life and Highlighting Societal Significance in Home Care. Internal Medicine. https://doi.org/10.2169/internalmedicine.2881-23
Zaidi, S. R. H., & Sharma, S. (2024, January 3). Pressure ulcer. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK553107/
